Bone Marrow Transplants and Stem-cell Transplants
At times, very advanced and nonresponsive lymphomas may be treated using a bone marrow transplant (marrow is the soft tissue in the centre of large bones that produces white and red blood cells and platelets) or stem-cell transplantation (the cells that develop blood).
Transplants fall into three basic donor categories:
A syngeneic transplant is when the cells are donated by an identical twin. Allogeneic is when the donor’s basic cell is almost identical to the patient’s as with a close relative (brother or sister). Rarely is the basic cell type matched by an unrelated relative.
Autologous is when the patient’s own stem cells are removed from his or her bone marrow or bloodstream. With types of NHL that have spread to the bloodstream or bone marrow, it may be difficult to obtain uncontaminated cells or cells that can be used, even after treating them in a laboratory to remove or kill the NHL cells.
Marrow or cell transplantation is done to replace healthy cells that have been destroyed by cancer treatment. Bone marrow or stem cells that have been removed from a donor are carefully frozen and stored while the patient receives high-dose chemotherapy and sometimes whole-body radiation treatment. This process kills all or most normal stem and bone marrow, while destroying cancer cells. This leaves them defenseless against infection and unable to form blood. After therapy, the frozen marrow or cells are thawed and put back in the body. During the recovery period, all of the body’s systems must be carefully monitored for rejection, infection and the need for any supportive treatments.
How do Stem-cell Transplants Work?
Stem cells, because they divide rapidly, can be killed off by chemotherapy and radiation therapy. Therefore, the doses of chemotherapy and radiation therapy used to treat lymphoma are limited due to the risk of damaging these stem cells. Patients with lymphomas that are difficult to treat or resistant to standard therapy may benefit from chemotherapy or radiation therapy given in very high doses (myeloablative therapy). However, this can potentially destroy all the stem-cells in the bone marrow and leave the patient at very high risk for infection. To combat this problem, the patient receives a bone marrow or a stem-cell transplant. This means that they receive stem cells (either their own stem cells that were stored prior to myeloablative therapy or stem cells from a donor) to replenish their bone marrow which had previously been destroyed by the high-dose therapy.
What is the Difference Between a Bone Marrow Transplant and a Stem-cell Transplant?
There are two different types of transplants: bone marrow transplants and peripheral blood stem-cell transplants (PBSCTs). The difference between the two depends on where the stem cells are taken from. In bone marrow transplants, the stem cells are taken from the bone marrow. In PBSCTs, the stem cells are taken from the circulating blood. PBSCTs are now more commonly performed than bone marrow transplants, as the procedure is easier and the body is able to regenerate new stem cells faster.
How are Transplants Performed?
Four steps are involved in a bone marrow transplant or PBSCT:
1. Harvesting stem cells or bone marrow: Harvesting is the procedure by which the bone marrow or stem cells are obtained in preparation for the transplant. In a bone marrow transplant, the stem cells are withdrawn from the bone marrow under general anesthesia by inserting a needle into a bone in the pelvic region, called the iliac crest. This bone marrow is then filtered and stored until the day of the transplant. In a PBSCT, stem cells are taken from the bloodstream, a far easier and more commonly used procedure. The stem cells are separated from other components of the blood in a process called apheresis, with the rest of the blood being returned to the patient.
2. Processing/preserving the stem cells or bone marrow: Stem cells or bone marrow harvested from the patient (autologous transplant) are generally preserved and stored in a freezer until ready for use. Stem cells or bone marrow derived from a donor (allogeneic transplant) are usually collected immediately before use and not stored for any length of time.
3. Administering myeloablative therapy: High-dose chemotherapy, with or without myeloablative radiation therapy, is then administered to the patient to destroy the cancerous cells, as well as the healthy cells in the bone marrow.
4. Reinfusing harvested stem cells or bone marrow: The harvested stem cells or bone marrow (obtained from either the patient’s own healthy cells or from a donor) are then transplanted intravenously into the bloodstream of the patient. The stem cells travel through the body to the bone marrow where they settle and implant themselves. These stem cells slowly begin to produce new, healthy blood cells. Eventually, they will produce enough healthy cells to repopulate the whole bone marrow, replenishing all blood and immune cells. Before the immune system is able to regenerate, the patient is at an increased risk of infection and must be closely monitored. The patient may also be susceptible to bleeding complications.
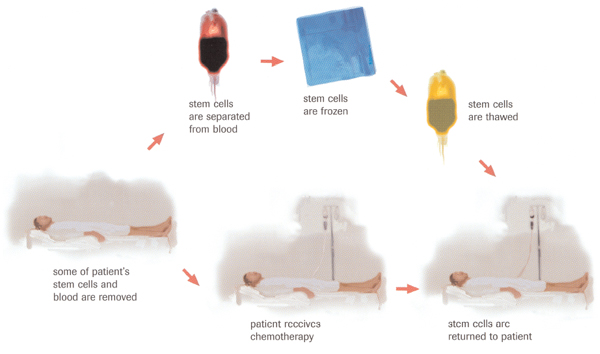
Autologous transplant
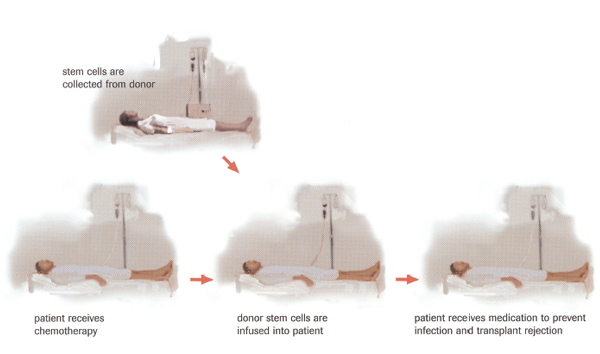
Allogeneic transplant